If there’s one book that I have been eagerly awaiting this year, it is unquestionably The Great Pretender by Susannah Cahalan (available Tuesday, November 5, 2019 from Grand Central Publishing). Part exploration of the Rosenhan experiment, part look at the history of psychiatry and how we got to where we are now, it is absolutely nothing short of brilliant, eye-opening, informative and engaging. In other words, a definite must-read. Last month, I had the opportunity to chat with her about how this book came about, David Rosenhan and his experiment, how labels can shape the way medical professionals treat and react to patients, the impact that the Rosenhan experiment had on the Diagnostic and Statistical Manual of Mental Disorders — also known as the DSM — and much more. Read on to see what she had to say…

Andrew DeCanniere (AD): To begin at the beginning, I was wondering when and how you decided to write this book or tackle this subject, in particular.
Susannah Cahalan (SC): It was on my paperback tour for Brain on Fire. It kind of took off in this unexpected way and I did not see it coming at all. I started becoming inundated with email from readers, and started to get access to some stories that I hadn’t really heard before. I was very obsessed with the autoimmune field and autoimmune encephalitis. As my story started to expand outside of that community, I started to hear other people’s stories. One of the emails I received was from a man whose son had been diagnosed with serious mental illness for the bulk of his adult life, and he very much related to Brain on Fire and saw it as a hopeful story. When he heard me talk about it — there was some kind of a book event and it was recorded — I started to make these hardline differences between my illness and psychiatric conditions. One was neurological and one was psychiatric. One was in the mind, one was in the brain. I was kind of making these unfair distinctions, and I think it really hurt his feelings. I was kind of using the same terminology that medicine uses. I was falling prey to the same trap that I think medicine falls prey to. Becoming aware of that fact made me uncomfortable, but it also made me want to examine that.
Around that same time, I visited a psychiatric hospital to talk about my experience because, at that point, I was lecturing everywhere I could to tell people about autoimmune encephalitis. When I was finished with my talk, one of the doctors came up to us and said ‘I think we have someone here who has this.’ I found out later that they did, but the woman had been misdiagnosed for years and would never recover the way I had. So, I started to ask ‘How are we getting this so wrong?,’ ‘What does it mean to have schizophrenia or serious mental illness if we are able to get it so wrong?,’ ‘What are the differences between what I went through and someone who lives with chronic schizophrenia?’
There were all of these questions over where the overlap exists among these illnesses and where my place was in history. It really galvanized my question to understand my own experience more. I think it started from there. Then, I was introduced to David Rosenhan’s study. I started to see so much of my own experience there that I became entirely obsessed with his story, and with the stories of the other pseudopatients. So, it led me down an entirely different path. It was definitely borne out of something personal, but it became something entirely different.
AD: Right. I think that, as a society, we really do tend to make those distinctions between a physical and mental illness. Even though I would think that the vast majority of people wouldn’t fault anyone for a psychiatric condition they may have, I do think that we do have this firm line drawn between the two.
SC: Exactly. Where, in reality, there is a very fuzzy line that we don’t quite understand. I’m not saying these lines don’t exist. All I’m trying to say is that there is a lot we don’t know, and drawing these hard lines can be very dangerous.
AD: And it almost seems like the more research is done — and the more that is discovered — it almost reinforces that we really aren’t even aware of just how much we don’t know or don’t understand.
SC: One hundred precent. Yes.
AD: As you illustrate in your book, it seems there have been many times throughout history where people were absolutely convinced that mental illness stems from this, that or the other. They could not be dissuaded, for whatever reason. Yet, over time, it came out that these people who were so certain that they had pinpointed the cause of these various psychiatric conditions could not have been further off the mark.
SC: Exactly.
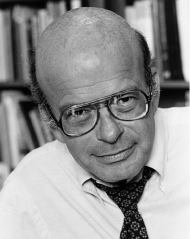
AD: And I know that, prior to reading your book, I certainly hadn’t heard of David Rosenhan or his experiment. So, I was wondering if you could also give a brief overview of who he was, what it was about, et cetera.
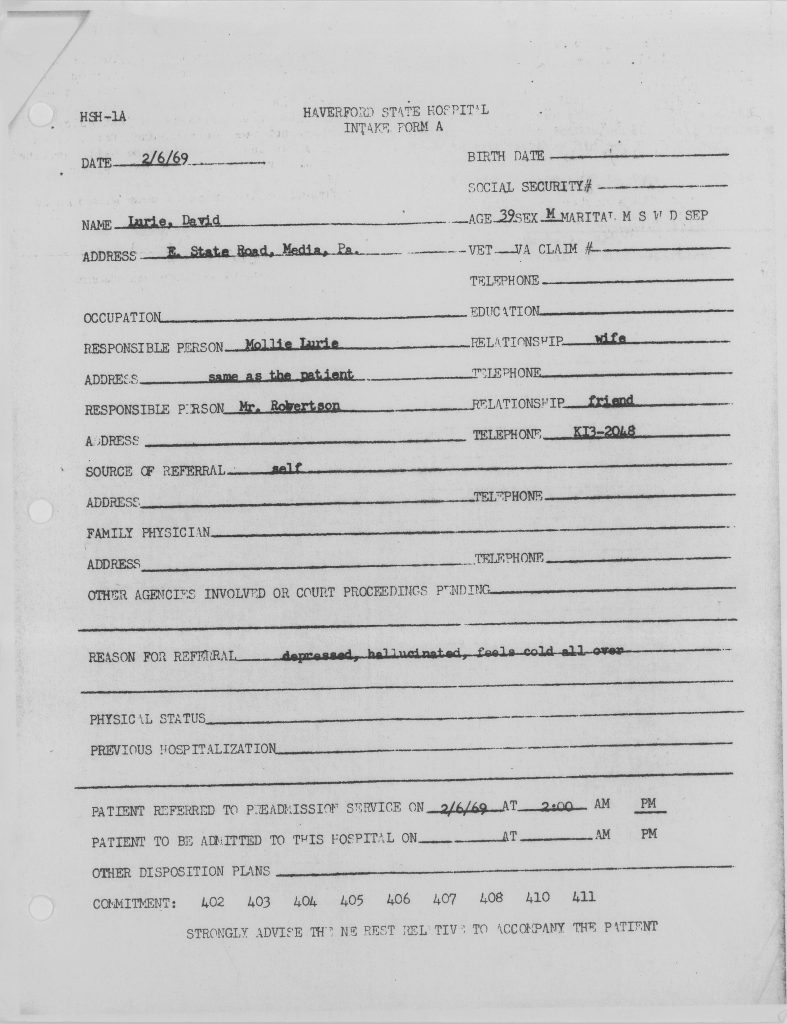
SC: I’d be happy to. So, the study itself was this kind of experiment where these eight people went undercover in psychiatric hospitals across the country to test the nature of diagnosis, and to report back about their experiences in these hospitals. The results were astounding. It’s so hard to talk about the book, because you always have to hedge things, but let’s say that we believe the paper as it stood, and each person told doctors they heard a voice that said ‘Thud,’ ‘empty’ or ‘hollow,’ and, based upon that alone, they were all diagnosed with serious mental illness. Seven were diagnosed with schizophrenia. One was diagnosed with manic depression, which was kind of a stand-in for bipolar disorder at the time. It became this sort of question of how you prove your sanity once you have been labeled insane. At the end of the day, I think that the average stay was 19 days, and one person was in for as long as 52 days. They all left the hospital against medical advice. So, none of these so-called ‘normal,’ healthy volunteers were ever seen as such.
Once they had been given that label of schizophrenia, for example, that label stayed with them the entire time — even though they dropped any sort of symptoms, and behaved as normally as they possibly could within hospital walls. There were so many things I related to so deeply in reading that paper — especially those first reads. One was the depersonalization — how, as a psychiatric patient, you were kind of treated, as David Rosenhan had put it, as a ‘netherperson.’ As kind of less human. At one point, David Rosenhan was made to strip with the door open, with no thought as to his modesty, or whether it would make him uncomfortable.
Patients were referred to almost as if they were prisoners — not necessarily by their numbers, but were disregarded. At one point the describes how one nurse started to adjust her bra in front of a room of male patients. It wasn’t as if she was trying to do it to get attention or to be seductive. She just didn’t care because they were not viewed as people, so she felt she could just do anything she wanted. She didn’t care. The bathroom stalls didn’t have any doors. There was a mess all over the floor that nobody would clean up because there was this attitude of ‘Who cares? They’re just patients,’ you know? There was this real palpable sense of the ‘othering’ of being mentally ill.
[Rosenhan] describes the cold and distant treatment the staff exhibited towards the patients, and I remember experiencing a little bit of that myself. That changed the minute my diagnosis became neurological. I also thought there was something very interesting about the idea of how labels shape the way we see the world. One of the great parts of that paper is the description of the pseudopatients writing — because they all wrote in journals while they were there, in order to take notes on the ward. In a few cases there was some documentation in nurses’ notes, to the effect of ‘patient engaging in writing behavior.’ So, the writing became a sign of their pathology, which is humorous in a way, but I actually experienced that, too. At one point, I had one of the psychiatrists who saw me describe my outfit — which was just leggings and a white T-shirt — as revealing because, in her mind, that was a sign of hyper sexuality that could support her diagnosis of Bipolar I. I related very deeply to those parts of the paper.
AD: It really is eye-opening and, when you think about it, it really is very odd how they pathologize things that, in any other context, would be unremarkable — whether you are talking about what you are wearing, or whether it is something as simple and quite ordinary as writing.
SC: Unremarkable is the key word there. You wouldn’t remark upon someone taking notes in a coffee shop, would you? Take that same person and throw them into a psychiatric hospital, and all of a sudden those notes become a sign of their psychosis.
AD: Right. The whole thing is just very strange because, as you allude to yourself, if someone had cancer or heart disease or diabetes or whatever else, I don’t think you’d have any less empathy for that person. Yet, somehow, when someone exhibits signs of psychosis, some people seem to take it as some kind of green light to not be empathetic anymore.
SC: I know. It’s something I still don’t fully understand. I think there are great minds who’ve kind of thought about this, but I still haven’t wrapped my mind around it. First, I think there’s something scary about psychosis. It’s scary for the person experiencing it and it can be scary to be around it. There’s something scary about not sharing the same reality as someone else. And I don’t know what you think about this, but I have thought about it, and maybe there is a sense of fear because w all know that all of us have straddled the line — because there is a continuum, right? We’ve all crossed the line off into a little bit of pathology, a little bit of dysfunction. Every single one of us, at some point in our lives, has at least stepped a toe over that line. So, maybe we all feel like we are capable of losing control as well. Maybe that makes it harder [for people] to empathize, because we’re scared it could happen to us, too. I don’t know.
AD: Right. Obviously, it’s hard to get into someone else’s head, but I think you’re onto something there. Even if you can’t be sure it will never happen to you — certainly no more certain than you will never have heart disease or diabetes or cancer or whatever else it may be. You can’t be 100 percent certain something like that won’t happen. So, maybe people do act like that because, as you’re saying, they can kind of imagine it happening to them. So, maybe it is borne — at least in part — out of fear. I certainly think people do go through ups and downs in life, and perhaps something like that is, for some people, too close for comfort. It’s just very hard, because I feel like it’s all so speculative.
SC: Exactly. It’s hard. It’s a hard thing to parse out. I don’t have a prescription to fix it, because I don’t know a lot of the answers to the questions I raise in the book, but what I hope is that people are more comfortable engaging in these conversations after having read the book, getting a little insight into the history, getting a little insight into the controversies. Just being able to converse about these questions will hopefully open up a broader conversation. That’s kind of my hope with the book.
AD: In any case, I know that I personally cannot conceive of being any less empathetic toward someone in that kind of position than someone with any other sort of condition.
SC: I think that, as a society, we have a bad homeless problem here in the city. I’m certainly not saying every person who is homeless has mental illness, because that is not true. However, there is a good percentage of the people who live on the streets who suffer from serious mental illness. Sometimes I just think ‘What if those people were suffering from Alzheimer’s?’ There are a lot of debates here, but wouldn’t we have intervened in some way if this were happening on a grand scale? They’re really hard questions, but I do think about that a lot.
AD: Right. If someone were in their eighties and clearly disoriented, it is hard to imagine someone would be okay with them living on the street or under a bridge or something like that. Yet, in a way, that is what is happening. It’s just that it’s not happening to people who have Alzheimer’s. It’s happening to people who have psychological issues.
You also touch on how the way in which people are treated in healthcare facilities is very different. You say that there seemed to be more empathy among healthcare professionals for those who are diagnosed with an organic illness than a psychiatric illness.
SC: Obviously it’s on a case-by-case basis, and it’s not a universal experience but, in my experience, I definitely saw a change. What’s so interesting to me, and what I think this David Rosenhan study really illuminates, is the role that context, labelling and environment play in the medical relationship — whether it’s in a psychiatric hospital or not. These are issues that I think plague medicine. A lot of the time, doctors see their patients as their diagnosis. That can cloud a lot of clinical judgment. And that can cloud a lot of empathetic judgment, too — empathetic relation. So, I think it’s not just a problem within psychiatry. It’s a problem in medicine — seeing people just through their label or diagnosis.
AD: I agree. Even when it comes to smaller things. Not to compare, because I think one is more serious and one is going in for something fairly routine — like a well check-up — but I think a lot of people have come across a medical professional who is lacking in empathy, whether it’s going to a doctor or going to a dentist or what have you, where there really doesn’t seem to be concern for your comfort or concerns or anything. It’s literally about getting you in, doing what they have to do, and then getting you out of the door as fast as possible.
SC: Yes. That’s the sad and sorry state of medicine in this country. And that’s not just psychiatry. It’s medicine in general.
AD: Thankfully, in my case, I was able to find someone who I feel is more capable than my previous dentist and, on top of that, manages to be concerned with you as a whole person. That said, I do think that too many medical professionals do seem to remove the person from the problem.
SC: Well, I am happy that you were able to do that on your own volition. One of my goals of this book is it enables others to do that, too. To say ‘I’m not being treated as a whole person,’ as you experienced — whether it’s a doctor or a dentist or a cardiologist or a psychiatrist — ‘I want to find someone else.’ Or else, ‘I demand to be treated a certain way.’ If someone feels like they’re being marginalized, or like they are being ignored or seen only through the prism of their label, I hope it gives them the power to question that — and to fight against that and to find someone that doesn’t do that. There are bad doctors [out there] and there are great doctors.
AD: Absolutely. I don’t want to demonize everyone.
SC: No. Of course not.
AD: But it does seem to be a pretty significant and persistent problem — even in this day and age, when we sort of think we’re all so enlightened — especially when it comes to those fields.
SC: You know, doctors are humans, and bias and context and labelling has a role in all of our lives, day-to-day. So, it is going to creep into the diagnostic language and the way in which doctors see their patients. Again, the goal of this book is making people aware — not just the doctors, but also the lay public — that this is a phenomenon that happens, and to make sure they armor themselves against that, too.
AD: One of the other things you touch upon, which I found to be of interest, is the story of Nellie Bly. I’m not sure if people are aware of how far back these problems with psychiatric facilities actually go. And you touch on that a little bit in recounting the story of Nellie Bly, who went undercover in order to report on the conditions of psychiatric facilities at that time. So, I think that, in many ways, we’ve come a long way from where we were — not to say things are perfect. Things are, in fact, still far from perfect.
SC: No, but in many, many ways we’ve come lightyears away from there. But in some ways we haven’t. Very seriously mentally ill people end up in prisons and jails to this day — in grotesque, horrific situations and environments that are not conducive to healing. They are the last place they should be — and places that do look a little bit like some of the things that Nellie Bly described about Blackwell’s Island. So, that was actually horrifying to me, when I got to really understand the issues with the criminal justice system and mental illness. When I really started to pull back the layers of that and interview people who’ve devoted their lives to exposing the atrocities there, I was horrified to find out how we haven’t advanced as much as we think we have.
AD: You also say that certain segments of the population — like people of color, for example — are significantly more likely to find themselves in jail or prison with mental illness.
SC: Definitely. And it’s a huge problem across the board in this country. I feel like that’s one of the problems that needs to be rectified as quickly as possible — to reform the criminal justice system and, from my perspective, to make sure that very seriously mentally ill people don’t end up in jail in the first place.
AD: I obviously don’t want to call them ‘success stories,’ because a ‘success story’ would be having facilities that are appropriate for people with these conditions and are fully able to care for them in the proper and compassionate way and really get them on their feet again. However, you do talk about some — like Cook County, here in Illinois — and how they’ve adapted as much as is possible for that environment to adapt to care for people who do have mental illness.
SC: Right. I do think that they’re being honest about their role. I think that’s what’s missing from a lot of the way that we’re treating these issues. A lot of jails and prisons don’t want to acknowledge that their role now is custodian to people who are very sick. I think that instead of denying it, Cook County met it head-on and really adapted the way that they treat people there with serious mental illness. They’re kind of game changers in that. I think if things are going to change, you have to first acknowledge the problem, and Cook County is doing extraordinary work in acknowledging that problem. I also think that there are communities that are making strides and are making sure that people who have serious mental illness don’t end up in prisons and jails to begin with. I think that’s really the work at the ground level.
AD: Right. I think it’s great, because being proactive and keeping them out of jails and prisons is even better than being reactive. Adapting jails and prisons to meet the needs of the mentally ill who unfortunately find themselves there is great. It’s a great first step. However, preventing them from ending up there in the first place is, as you say, the ultimate goal.
SC: I agree with you completely.
AD: You also talk about how Rosenhan’s study had this profound impact on psychiatry and, it seems, one of the ways it impacted the field is in how it impacted the DSM. It’s interesting to examine how it impacted psychiatry as a whole, really.
SC: I know. It is amazing to see how wide-ranging the effects of the study were. It really touched upon so many different movements that seem to have nothing in common. In some ways, it helped support the anti-psychiatry movement. It provided a lot of fodder for the anti-psychiatry movement, while also supporting the deinstitutionalization movement. It kind of provided proof that not only don’t these institutions know how to tell a sane person from an insane person, ad David Rosenhan would write, but also are harmful places. On top of that, it also contributed to a push to rebrand psychiatry and refocus it — and to take a more scientific, biological approach, so that embarrassments — like this Rosenhan study — would never happen again.
You know that, in the book, I detail the back-and-forth between David Robenhan and Robert Spitzer, who is the architect of the DSM-III, and the ways in which David’s study really did affect Spitzer’s way of thinking about how to structure his diagnostic system to make sure these pseudopatients wouldn’t get past him again. It was amazing to see the real aftershocks of this study. I describe it as kind of these tentacles coming off of it. You would think that this one study, which was really a demonstration — it wasn’t an experiment. It was kind of anecdotal, even though it had a lot of data, which I think made it different than any of the people who had gone before. It was the first time someone actually put hard numbers [together] with these philosophies and thoughts. But you would think it would be a kind of a fad and that it would disappear. However, I think because it was published in Science — which is such an important scientific journal — it had a huge effect. And its effect is still being seen today.
AD: Right. And, in the wake of Rosenhan’s study, I think the DSM-III almost overcompensated.
SC: I think you’re right.
AD: As you say in your book, it seems that there is even some acknowledgment of that from the man behind the DSM-IV in his critique of the DSM-5.
SC: I think so. Of course, there will always be DSM hardliners. The DSM was created as a living document, which is why there are new editions. At the point they were writing it, there was still so much unknown. In a way, I love that about the DSM. In the best interpretation of that document, it’s an acknowledgment that we’re just at the very beginning of the understanding of these issues. You know, there were a bunch of people sitting in a room and this was their best attempt to make sense of this. But what happened was, there was this kind of diehard belief in the DSM as having these hard lines — [and] you have these hard line differences among these diagnoses that maybe weren’t really intended to be so extreme.
The book is so prescribed and that’s one of the major downsides of the DSM according to that people I’ve talked to about it. It’s hyper-organized, and everything is [this sort of] checklist system. It has no room for an acceptance of the unknown. It has no room for nuance. Each patient is different, even if you are talking about someone who has cancer. Not every person who has colon cancer is going to respond the same way to the same drugs. In the same way, not everyone who is diagnosed with schizophrenia looks anything like another person diagnosed with schizophrenia. It doesn’t really acknowledge the gradients of all these things and the gray areas. I think that was a huge mistake, but I think that in many ways it was a reaction to the Rosenhan study.
AD: Absolutely. As you say, I think if you look at something like cancer, there are certainly branches of medicine that are looking at your genes — your DNA — and how to create treatments that are specifically tailored to you, individually. Yet, on the other hand, you do have people like this guy who is a psychiatrist, who asked you something to the effect of ‘So, what do schizophrenics think of the book?’ It just seems to me that a question like that suggests that he does see them all one way.
SC: Absolutely. That was appalling to me. That was an exceptional example, but it happened. And this is someone who works with people who have serious mental illness for his career, and he studies people. It was really gross, but also indicative of the way some people do feel about their patient population.
AD: And, interestingly, that’s the same guy who seemed to be pushing back against the idea of any sort of reforms.
SC: I always wondered what really bothered him. You know, psychiatry had a bad rep. A lot of the times, deservedly so. It has a really horrible history. However, all of medicine has a really dark history, and I think that what psychiatry does is really hard. The best psychiatrists are the ones who acknowledge the limitations and work within what they have and can tell you ‘We don’t know, but this is the best practice that we can figure out.’ I think that with Brain on Fire, he saw me as a sign of advancement and then, with this book, he saw me as someone who is going to push back against that advancement, or maybe push back against psychiatry. I don’t know. It was just an interesting take on my being interested in this study. It was like how dare I even find the study compelling at all? Because he was so afraid of my going in an anti-psychiatry way. So, I think there was a lot of fear there.
AD: Yeah. I don’t get it. Personally, I think that it is only through doing precisely what you are doing with this book — through writing about it, talking about it, challenging it, looking into it— that things are going to get better. I really do believe that by doing what you are doing, by looking into it as you have, you are pushing the field to do better and to make advancements.
SC: Thank you. That is the goal. I do think that, in exposing the study for the problems that it has — and I know we’re not going to go too far into that here — but, in some ways, some psychiatrists could see that as a kind of ‘Look. See? This study that embarrasses wasn’t even true.’ You know? But I do also think that it does push back against this narrative of ‘Look how far we’ve advanced.’ I think psychiatrists [and others] would kind of prop the study up by saying ‘Look, it would never happen today.’ But now that we find out the study wasn’t as clear-cut, it really doesn’t give you the opportunity to say ‘Look how far we’ve advanced since then.’
AD: And I think that, generally speaking, you really do tend to make bigger advances by pushing back and by challenging the status quo than by sitting silently and idly by.
SC: Yeah. There’s this quote from Daniel Boorstin that I use in the book: ‘The greatest obstacle to discovery is not ignorance — it is the illusion of knowledge.’ It’s inserting knowledge where we don’t have it and not accepting the fact that we don’t know. Because, actually, it should be exciting. I understand that for people on the ground level, treating very seriously sick people, it’s hard to have this perspective — but for people in research, I think it should be exciting to know how little we know. That’s how much progress we can make.
If you kind of switch it around, and instead of being scared and frightened by this, I hope that people are kind of excited by it and galvanized by it. I think there are groups of younger psychiatrists and neurologists — and a lot of people who bridge the two, who do psych and neuro together, which I think is very exciting — I think they actually are excited by the limitations because don’t you want to look back, 50 years from now, at this time and think ‘Look how barbaric that was. Look how primitive our instruments were, and the tools we used and the terms we used. Wasn’t that so primitive?’ Of course we want that, you know?
AD: Right. If you’re in the field, you would think you would want to be able to say ‘I was a part of that change.’
SC: I think that a lot of the younger people are all aboard on that. I think that there are maybe some of the old guard who feel a little protective, because I think there was a lot of research — and a lot of excitement — and a lot of it didn’t go anywhere. It didn’t come to fruition because these are hard — or impossible — questions. It’s not anyone’s fault. It’s just that these are really difficult questions. But I think there’s a little bit of a turf thing, where people have spent their whole lives studying, say, the genetics of schizophrenia and it never quite led to the breakthrough they’d hoped. A lot of people who I’ve talked to who devoted their lives to imaging and genetics will say ‘I might have been too targeted with what I was focusing my research on.’ I heard a lot of people talking about their careers and they were kind of saying ‘You know, I should have been looking more at epigenetics. I should’ve been looking more at environment.’ So, it’s an interesting thing once people are looking back — but not everyone has that perspective. Some people want to defend their turf, their legacy, which is understandable. I get it.
AD: Sure. I’d guess it can be unpleasant to have your work questioned and yet, as you say, it’s only through asking the questions that things can get better.
SC: Exactly.
AD: So, I guess there’s this push and pull kind of thing. What I also found interesting, when it comes to the Rosenhan study, is this one experience of one of the pseudopatients and how he seems to have reacted to it. There was one guy who participated in the study and, it would seem, he came away with a completely different take on these psychiatric facilities. He actually had what seem to be rather pleasant experiences while there, and so he had this sort of positive takeaway from the whole thing. And it really did seem that, perhaps because of that, Rosenhan didn’t really seem to want to include it in his study.
SC: Yeah. That was pretty alarming when I found that. I went with Harry’s assessment — which was that his experience didn’t fit [Rosenhan’s] thesis, so he discarded the data. That felt very unscientific and unfair. I really feel Harry could have added a layer of nuance to his article and an argument that may have changed some of the debate over these issues. Even David’s study took some hardline approaches that perhaps weren’t fair. I think that Harry could have given him the opportunity to draw that out, and he didn’t use that. I really think we’ve suffered from that — but I think that the study itself had suffered, too.
AD: Right. As you say, it would have been a more three-dimensional picture, in terms of what was going on in these facilities at that time. Another interesting point of note was that he perhaps wasn’t quite as careful with the pseudopatients involved in the study as might have been thought or assumed. For instance, just even in terms of the planning. In a way, I don’t want to sound judgmental, but he doesn’t seem to have been particularly careful in training the pseudopatients, for example.
SC: No. For example, I found out that [one of the pseudopatients], Bill — who I talked to first — swallowed Thorazine. It would rapidly melt [in patients’ mouths] and burn so that people would swallow it. Wouldn’t that be something you’d want to look into, [in order to] make sure you aren’t letting your students take very serious psychopharmaceuticals? And then there was the whole mix-up about the hospital with Harry. They hadn’t even vetted the hospital he went into, because they had the wrong catchment area. So, there wasn’t a lot of preparation for the pseudopatients that I found — which showed a kind of haphazard way and a lack of diligence, where I started to question other parts of the paper, too.
AD: Yeah. And then there was that whole thing about the writs of habeas corpus. He seemed to have suggested that he had papers drawn up and ready to go, if need be, but then it seems like he may not have done any such thing. There may not have been anything ready to go after all.
SC: Yeah. Maybe he talked about it, but he didn’t have them ready to go. It’s always like a slight variation. So, you know, everything is a little cockeyed. Everything is a little bit off. Most of the things that happened weren’t exactly as he said they did.
AD: And, as you you seem to say, you’re sort of left with this question of ‘Was it really because he was so concerned with the privacy and anonymity of the pseudopatients? Or is it because some of it either didn’t happen or else didn’t happen the way that he said it had happened?’
I mean, I think it’s possible at least some portion of it was made up — especially since you touch on the fact that these kinds of things happen to this day, where people fabricate at least parts of studies or manipulate them in some fashion. And, as you say, it may happen even more today, because there are fewer of these coveted positions that many of these people who conduct these studies are competing for. So, if it’s happening now, it’s certainly possible it was happening back then.
SC: And it was easier back then. Now there are greater numbers of people being caught in these kinds of lies. Back then you didn’t have that. Now there’s skepticism that I think is applied across the board — not just with psychology and psychiatry.
AD: And, I would say, that it is largely because when these kinds of things came to light — even in the seventies, at least within the field — I think that may have been what drove at least part of the skepticism that we now feel today.
SC: Definitely. I think that a lot of those studies that were borne out of that time were very loose. You didn’t need review boards, which you need now. There was a lot more leeway and sometimes people even took it to another extreme. There have been cases of that, but the fact that a lot of these studies have now been reassessed and, in some cases, kind of rejected as being not entirely truthful or somewhat fraudulent. It’s important, I think, because a lot of these studies were foundational studies. They had huge effects on the kind of building blocks of their field — in social psychology, especially. So, even though these studies may be 40 or 50 years old, it’s really important we figure out what was real about these studies and what wasn’t.
AD: Right. And anyone can really say anything about anyone. I mean, someone could have a good opinion of someone and another person could have a bad opinion of someone, and we could be talking about the same person. So, one person’s opinion of somebody doesn’t definitely prove or disprove anything. So, not that it is definitive proof that he fabricated part or all of the study, but it is interesting that there was that one person in your book who suggested Rosenhan had a tendency to avoid work. And a study of this sort seems like it would have been a significant amount of work. So, that was kind of another red flag to me. I just felt like that didn’t bode particularly well for him.
SC: No. There were a lot of things in his personal life. As I started getting drawn into his story, it became impossible to separate his personal life from the study. I had to go into his personal life and figure out who he was — you know, his career but also his family life. All of those things became part of the story in trying to figure him out and what he was capable of.
AD: And I do think that’s so hard to pin down, because he seems very chameleon-like, if you will.
SC: Which is very appealing in some ways. It’s a hard person to write about, but very appealing in some ways. He’s an extremely compelling character.
Susannah Cahalan is the award-winning, New York Times bestselling author of Brain on Fire: My Month of Madness, a memoir about her struggle with a rare autoimmune disease of the brain. She writes for the New York Post. Her work has also been featured in the New York Times, Biological Psychiatry, Scientific American magazine, Elle, Psychology Today, and other publications. She lives in Brooklyn.
For more information about Susannah and her work, visit her website.
In addition, you can find my 2013 interview with Susannah regarding her memoir, Brain on Fire: My Month of Madness, by clicking here.

Be the first to comment